You are looking for information, articles, knowledge about the topic nail salons open on sunday near me 심방 세동 치료 가이드 라인 on Google, you do not find the information you need! Here are the best content compiled and compiled by the https://toplist.pilgrimjournalist.com team, along with other related topics such as: 심방 세동 치료 가이드 라인 심방세동 완치율, 심방세동 관리, 심방세동 응급처치, 심방세동 심부전, 심방세동 진단기준, 심방세동 종류, 심방세동 심전도, Atrial fibrillation Guideline
Table of Contents
2021 ëíë¶ì 맥íí ì¬ë°©ì¸ë íìì ëì¡¸ì¤ ìë°© ê´ë¦¬ ì§ì¹¨
- Article author: www.ekjm.org
- Reviews from users: 46721
Ratings
- Top rated: 4.1
- Lowest rated: 1
- Summary of article content: Articles about 2021 ëíë¶ì 맥íí ì¬ë°©ì¸ë íìì ëì¡¸ì¤ ìë°© ê´ë¦¬ ì§ì¹¨ 2021 대한부정맥학회 심방세동 환자의 뇌졸중 예방 관리 지침. 2021 Korean Heart Rhythm Society Guelines for Stroke Prevention in Atrial … …
- Most searched keywords: Whether you are looking for 2021 ëíë¶ì 맥íí ì¬ë°©ì¸ë íìì ëì¡¸ì¤ ìë°© ê´ë¦¬ ì§ì¹¨ 2021 대한부정맥학회 심방세동 환자의 뇌졸중 예방 관리 지침. 2021 Korean Heart Rhythm Society Guelines for Stroke Prevention in Atrial …
- Table of Contents:
Article information
Trans Abstract
ì ë¡
본 ë¡
ê²° ë¡
Acknowledgements
References
Article information Continued

:: JKMA :: Journal of the Korean Medical Association
- Article author: jkma.kr
- Reviews from users: 3065
Ratings
- Top rated: 3.4
- Lowest rated: 1
- Summary of article content: Articles about :: JKMA :: Journal of the Korean Medical Association 심방세동 치료 가이드라인. 정보영. 연세대학교 의과대학 세브란스병원 심장내과. Gueline of atrial fibrillation management. Boyoung Joung , MD. …
- Most searched keywords: Whether you are looking for :: JKMA :: Journal of the Korean Medical Association 심방세동 치료 가이드라인. 정보영. 연세대학교 의과대학 세브란스병원 심장내과. Gueline of atrial fibrillation management. Boyoung Joung , MD.
- Table of Contents:

:: JKMA :: Journal of the Korean Medical Association
- Article author: health.chosun.com
- Reviews from users: 37492
Ratings
- Top rated: 3.9
- Lowest rated: 1
- Summary of article content: Articles about :: JKMA :: Journal of the Korean Medical Association 대한부정맥학회는 최근 ‘2018 심방세동 카테터 절제술 대한민국 진료지침’ 개정판을 내고, 국제학술지(International Journal of Arrhythmia)를 통해 공개 … …
- Most searched keywords: Whether you are looking for :: JKMA :: Journal of the Korean Medical Association 대한부정맥학회는 최근 ‘2018 심방세동 카테터 절제술 대한민국 진료지침’ 개정판을 내고, 국제학술지(International Journal of Arrhythmia)를 통해 공개 …
- Table of Contents:

심방세동 치료 가이드라인 : 네이버 블로그
- Article author: m.blog.naver.com
- Reviews from users: 44154
Ratings
- Top rated: 4.2
- Lowest rated: 1
- Summary of article content: Articles about 심방세동 치료 가이드라인 : 네이버 블로그 심방세동 치료 가이드라인. Gueline of atrial fibrillation management. . 정보영 | 연세대학교 의과대학 세브란스병원 심장내과. …
- Most searched keywords: Whether you are looking for 심방세동 치료 가이드라인 : 네이버 블로그 심방세동 치료 가이드라인. Gueline of atrial fibrillation management. . 정보영 | 연세대학교 의과대학 세브란스병원 심장내과.
- Table of Contents:
카테고리 이동
DrKim’s Anestopia
이 블로그
마취전 평가관리
카테고리 글
카테고리
이 블로그
마취전 평가관리
카테고리 글
심방세동 치료 가이드라인
- Article author: www.kci.go.kr
- Reviews from users: 40356
Ratings
- Top rated: 3.6
- Lowest rated: 1
- Summary of article content: Articles about 심방세동 치료 가이드라인 키워드열기/닫기 버튼 ; 심방세동 ·, ; 지침 ·, ; 항응고 ·, ; 치료 · Atrial fibrillation, Gueline, Anticoagulants, Therapy … …
- Most searched keywords: Whether you are looking for 심방세동 치료 가이드라인 키워드열기/닫기 버튼 ; 심방세동 ·, ; 지침 ·, ; 항응고 ·, ; 치료 · Atrial fibrillation, Gueline, Anticoagulants, Therapy … Guideline of atrial fibrillation management – Atrial fibrillation;Guideline;Anticoagulants;Therapy
- Table of Contents:
초록
열기닫기 버튼
키워드열기닫기 버튼
인용현황
KCI에서 이 논문을 인용한 논문의 수는 1건입니다
열기닫기 버튼
참고문헌(16)
열기닫기 버튼
2020년 이후 발행 논문의 참고문헌은 현재 구축 중입니다

See more articles in the same category here: Toplist.pilgrimjournalist.com/blog.
2021 대한부정맥학회 심방세동 환자의 뇌졸중 예방 관리 지침
Correspondence to Jin-Bae Kim, M.D., Ph.D. Division of Cardiology, Department of Internal Medicine, Kyung Hee University Hospital, College of Medicine, Kyung Hee University, 23 kyungheedae-ro, Dongdaemun-gu, Seoul 02447, Korea Tel: +82-2-958-8167, Fax: +82-2-958-8160, E-mail: [email protected]
5 Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
4 Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea
Atrial fibrillation (AF) is a strong risk factor for ischemic stroke and systemic embolism. To prevent thromboembolic events in patients with AF, anticoagulation therapy is essential. The anticoagulant strategy is determined after stroke and bleeding risk assessments using the CHA 2 DS 2 -VASc and HAS-BLED scores, respectively; both consider clinical risk factors. Vitamin K antagonists (VKAs) are the sole anticoagulant option in AF patients with a prosthetic mechanical valve or moderate-severe mitral stenosis; in all other AF patients VKA or non-vitamin K antagonist oral anticoagulants are therapeutic options. However, antiplatelet therapy should not be used for stroke prevention in AF patients. Anticoagulation is not needed in AF patients with low stroke risk but strongly recommended in those with a with low bleeding risk. Left atrial appendage (LAA) occlusion offers an alternative in AF patients in whom long-term anticoagulation is contraindicated. Surgical occlusion or the exclusion of LAA can be considered for stroke prevention in AF patients undergoing cardiac surgery. In this article, we review existing data for stroke prevention and suggest optimal strategies to prevent stroke in AF patients.
오직 Watchman 기구만이 무작위 대조군 연구인 PROTECT AF (WATCHMAN Left Atrial Appendage System for Embolic Protection in Patients With Atrial Fibrillation) 연구와 PREVAIL (Watchman LAA Closure Device in Patients With Atrial Fibrillation Versus Long Term Warfarin Therapy) 연구에서 비타민 K 길항제와 비교되었는데, 뇌졸중 위험도가 중등도 이상인 환자군에서 좌심방이 폐색술은 비타민 K 길항제와 비교하였을 때 열등하지 않음을 보여주었고, 장기간의 추적에서도, 출혈 위험을 감소시킬 수 있는 것으로 나타났다[ 82 – 85 ]. 항응고 치료의 금기증에 해당하는 환자들에서 좌심방이 폐색술은 뇌졸중 위험도도 낮추어 줄 수 있는 것으로 나타났다[ 83 , 86 ].
References
1. Pisters R, Lane DA, Marin F, Camm AJ, Lip GY. Stroke and thromboembolism in atrial fibrillation. Circ J 2012;76:2289–2304.
2. Szymanski FM, Lip GY, Filipiak KJ, Platek AE, Hrynkiewicz-Szymanska A, Opolski G. Stroke risk factors beyond the CHA₂DS₂-VASc score: can we improve our identification of “high stroke risk” patients with atrial fibrillation? Am J Cardiol 2015;116:1781–1788.
3. Ganesan AN, Chew DP, Hartshorne T, et al. The impact of atrial fibrillation type on the risk of thromboembolism, mortality, and bleeding: a systematic review and meta-analysis. Eur Heart J 2016;37:1591–1602.
4. Allan V, Honarbakhsh S, Casas JP, et al. Are cardiovascular risk factors also associated with the incidence of atrial fibrillation? A systematic review and field synopsis of 23 factors in 32 population-based cohorts of 20 million participants. Thromb Haemost 2017;117:837–850.
5. Banerjee A, Taillandier S, Olesen JB, et al. Ejection fraction and outcomes in patients with atrial fibrillation and heart failure: the Loire Valley Atrial Fibrillation Project. Eur J Heart Fail 2012;14:295–301.
6. Lee SE, Park JK, Uhm JS, et al. Impact of atrial fibrillation on the clinical course of apical hypertrophic cardiomyopathy. Heart 2017;10:1496–1501.
7. Shin SY, Han SJ, Kim JS, et al. Identification of markers associated with development of stroke in “clinically low-risk” atrial fibrillation patients. J Am Heart Assoc 2019;8e012697.
8. Kang SH, Choi EK, Han KD, et al. Risk of ischemic stroke in patients with non-valvular atrial fibrillation not receiving oral anticoagulants-Korean nationwide population-based study. Circ J 2017;81:1158–1164.
9. Jung H, Sung JH, Yang PS, et al. Stroke risk stratification for atrial fibrillation patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 2018;72:2409–2411.
10. Wu VC, Wu M, Aboyans V, et al. Female sex as a risk factor for ischaemic stroke varies with age in patients with atrial fibrillation. Heart 2020;106:534–540.
11. Tomasdottir M, Friberg L, Hijazi Z, Lindbäck J, Oldgren J. Risk of ischemic stroke and utility of CHA2 DS2 -VASc score in women and men with atrial fibrillation. Clin Cardiol 2019;42:1003–1009.
12. Friberg L, Benson L, Rosenqvist M, Lip GY. Assessment of female sex as a risk factor in atrial fibrillation in Sweden: nationwide retrospective cohort study. BMJ 2012;344e3522.
13. Overvad TF, Potpara TS, Nielsen PB. Stroke risk stratification: CHA 2 DS 2 -VA or CHA 2 DS 2 -VASc? Heart Lung Circ 2019;28:e14–e15.
14. Nielsen PB, Overvad TF. Female sex as a risk modifier for stroke risk in atrial fibrillation: using CHA 2 DS 2 -VASc versus CHA 2 DS 2 -VA for stroke risk stratification in atrial fibrillation: a note of caution. Thromb Haemost 2020;120:894–898.
15. Nielsen PB, Skjøth F, Overvad TF, Larsen TB, Lip GYH. Female sex is a risk modifier rather than a risk factor for stroke in atrial fibrillation: should we use a CHA 2 DS 2 -VA score rather than CHA 2 DS 2 -VASc? Circulation 2018;137:832–840.
16. Marzona I, Proietti M, Farcomeni A, et al. Sex differences in stroke and major adverse clinical events in patients with atrial fibrillation: a systematic review and meta-analysis of 993,600 patients. Int J Cardiol 2018;269:182–191.
17. Kim TH, Yang PS, Uhm JS, et al. CHA 2 DS 2 -VASc score (congestive heart failure, hypertension, age ≥75 [doubled], diabetes mellitus, prior stroke or transient ischemic attack [doubled], vascular disease, age 65-74, female) for stroke in Asian patients with atrial fibrillation: a Korean nationwide sample cohort study. Stroke 2017;48:1524–1530.
18. Kim TH, Yang PS, Kim D, et al. CHA 2 DS 2 -VASc score for identifying truly low-risk atrial fibrillation for stroke: a Korean nationwide cohort study. Stroke 2017;48:2984–2990.
19. Vinereanu D, Lopes RD, Mulder H, et al. Echocardiographic risk factors for stroke and outcomes in patients with atrial fibrillation anticoagulated with apixaban or warfarin. Stroke 2017;48:3266–3273.
20. Echocardiographic predictors of stroke in patients with atrial fibrillation: a prospective study of 1066 patients from 3 clinical trials. Arch Intern Med 1998;158:1316–1320.
21. Friberg L, Benson L, Lip GY. Balancing stroke and bleeding risks in patients with atrial fibrillation and renal failure: the Swedish atrial fibrillation cohort study. Eur Heart J 2015;36:297–306.
22. Poli M, Philip P, Taillard J, et al. Atrial fibrillation is a major cause of stroke in apneic patients: a prospective study. Sleep Med 2017;30:251–254.
23. Bassand JP, Accetta G, Al Mahmeed W, et al. Risk factors for death, stroke, and bleeding in 28,628 patients from the GARFIELD-AF registry: rationale for comprehensive management of atrial fibrillation. PLoS One 2018;13e0191592.
24. Overvad TF, Rasmussen LH, Skjøth F, Overvad K, Lip GY, Larsen TB. Body mass index and adverse events in patients with incident atrial fibrillation. Am J Med 2013;126:640.e9–640.e6.4E17.
25. Lee JM, Kim JB, Uhm JS, Pak HN, Lee MH, Joung B. Additional value of left atrial appendage geometry and hemodynamics when considering anticoagulation strategy in patients with atrial fibrillation with low CHA 2 DS 2 -VASc scores. Heart Rhythm 2017;14:1297–1301.
26. Baek YS, Yang PS, Kim TH, et al. Associations of abdominal obesity and new-onset atrial fibrillation in the general population. J Am Heart Assoc 2017;6e004705.
27. Kim TH, Shim CY, Park JH, et al. Left ventricular diastolic dysfunction is associated with atrial remodeling and risk or presence of stroke in patients with paroxysmal atrial fibrillation. J Cardiol 2016;68:104–109.
28. Hijazi Z, Oldgren J, Siegbahn A, Wallentin L. Application of biomarkers for risk stratification in patients with atrial fibrillation. Clin Chem 2017;63:152–164.
29. Lee KH, Shin MH, Park HW, Cho JG, Kweon SS, Lee YH. Association between serum parathyroid hormone levels and the prevalence of atrial fibrillation: the Dong-gu Study. Korean Circ J 2018;48:159–167.
30. Lip GY, Lane D, Van Walraven C, Hart RG. Additive role of plasma von Willebrand factor levels to clinical factors for risk stratification of patients with atrial fibrillation. Stroke 2006;37:2294–2300.
31. Chao TF, Lip GYH, Lin YJ, et al. Incident risk factors and major bleeding in patients with atrial fibrillation treated with oral anticoagulants: a comparison of baseline, follow-up and delta HAS-BLED scores with an approach focused on modifiable bleeding risk factors. Thromb Haemost 2018;118:768–777.
32. Man-Son-Hing M, Nichol G, Lau A, Laupacis A. Choosing antithrombotic therapy for elderly patients with atrial fibrillation who are at risk for falls. Arch Intern Med 1999;159:677–685.
33. Esteve-Pastor MA, Rivera-Caravaca JM, Roldan V, et al. Long-term bleeding risk prediction in ‘real world’ patients with atrial fibrillation: comparison of the HAS-BLED and ABC-bleeding risk scores. The murcia atrial fibrillation project. Thromb Haemost 2017;117:1848–1858.
34. Borre ED, Goode A, Raitz G, et al. Predicting thromboembolic and bleeding event risk in patients with non-valvular atrial fibrillation: a systematic review. Thromb Haemost 2018;118:2171–2187.
35. Caldeira D, Costa J, Fernandes RM, Pinto FJ, Ferreira JJ. Performance of the HAS-BLED high bleeding-risk category, compared to ATRIA and HEMORR2HAGES in patients with atrial fibrillation: a systematic review and meta-analysis. J Interv Card Electrophysiol 2014;40:277–284.
36. Chang G, Xie Q, Ma L, et al. Accuracy of HAS-BLED and other bleeding risk assessment tools in predicting major bleeding events in atrial fibrillation: a network meta-analysis. J Thromb Haemost 2020;18:791–801.
37. Zhu W, He W, Guo L, Wang X, Hong K. The HAS-BLED score for predicting major bleeding risk in anticoagulated patients with atrial fibrillation: a systematic review and meta-analysis. Clin Cardiol 2015;38:555–561.
38. Berg DD, Ruff CT, Jarolim P, et al. Performance of the ABC scores for assessing the risk of stroke or systemic embolism and bleeding in patients with atrial fibrillation in ENGAGE AF-TIMI 48. Circulation 2019;139:760–771.
39. Hijazi Z, Oldgren J, Lindbäck J, et al. The novel biomarker-based ABC (age, biomarkers, clinical history)-bleeding risk score for patients with atrial fibrillation: a derivation and validation study. Lancet 2016;387:2302–2311.
40. Lip GY, Lane DA. Bleeding risk assessment in atrial fibrillation: observations on the use and misuse of bleeding risk scores. J Thromb Haemost 2016;14:1711–1714.
41. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med 2007;146:857–867.
42. De Caterina R, Husted S, Wallentin L, et al. Vitamin K antagonists in heart disease: current status and perspectives (Section III). Position paper of the ESC Working Group on Thrombosis–Task Force on Anticoagulants in Heart Disease. Thromb Haemost 2013;110:1087–1107.
43. Choi WS, Kim JH, Jang SY, et al. Optimal international normalized ratio for warfarin therapy in elderly Korean patients with non-valvular atrial fibrillation. Int J Arrhythm 2016;17:167–173.
44. Lee IH, Kim H, Je NK. Underutilization of warfarin for stroke prophylaxis in patients with atrial fibrillation or atrial flutter in Korea. J Cardiol 2015;66:475–481.
45. Wan Y, Heneghan C, Perera R, et al. Anticoagulation control and prediction of adverse events in patients with atrial fibrillation: a systematic review. Circ Cardiovasc Qual Outcomes 2008;1:84–91.
46. Lee KH, Cho JG, Lee N, et al. Impact of anticoagulation intensity in Korean patients with atrial fibrillation: is it different from western population? Korean Circ J 2020;50:163–175.
47. Amin A, Deitelzweig S, Jing Y, et al. Estimation of the impact of warfarin’s time-in-therapeutic range on stroke and major bleeding rates and its influence on the medical cost avoidance associated with novel oral anticoagulant use-learnings from ARISTOTLE, ROCKET-AF, and RE-LY trials. J Thromb Thrombolysis 2014;38:150–159.
48. Själander S, Sjögren V, Renlund H, Norrving B, Själander A. Dabigatran, rivaroxaban and apixaban vs. high TTR warfarin in atrial fibrillation. Thromb Res 2018;167:113–118.
49. Proietti M, Lip GY. Simple decision-making between a vitamin K antagonist and a non-vitamin K antagonist oral anticoagulant: using the SAMe-TT 2 R 2 score. Eur Heart J Cardiovasc Pharmacother 2015;1:150–152.
50. Apostolakis S, Sullivan RM, Olshansky B, Lip GYH. Factors affecting quality of anticoagulation control among patients with atrial fibrillation on warfarin: the SAMe-TT₂ R₂ score. Chest 2013;144:1555–1563.
51. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009;361:1139–1151.
52. Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 2011;365:883–891.
53. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2011;365:981–992.
54. Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2013;369:2093–2104.
55. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet 2014;383:955–962.
56. Wang KL, Lip GY, Lin SJ, Chiang CE. Non-vitamin K antagonist oral anticoagulants for stroke prevention in Asian patients with nonvalvular atrial fibrillation: meta-analysis. Stroke 2015;46:2555–2561.
57. Cha MJ, Choi EK, Han KD, et al. Effectiveness and safety of non-vitamin K antagonist oral anticoagulants in Asian patients with atrial fibrillation. Stroke 2017;48:3040–3048.
58. Connolly SJ, Eikelboom J, Joyner C, et al. Apixaban in patients with atrial fibrillation. N Engl J Med 2011;364:806–817.
59. Camm AJ, Amarenco P, Haas S, et al. XANTUS: a real-world, prospective, observational study of patients treated with rivaroxaban for stroke prevention in atrial fibrillation. Eur Heart J 2016;37:1145–1153.
60. Carmo J, Moscoso Costa F, Ferreira J, Mendes M. Dabigatran in real-world atrial fibrillation. Meta-analysis of observational comparison studies with vitamin K antagonists. Thromb Haemost 2016;116:754–763.
61. Huisman MV, Rothman KJ, Paquette M, et al. Two-year follow-up of patients treated with dabigatran for stroke prevention in atrial fibrillation: global registry on long-term antithrombotic treatment in patients with atrial fibrillation (GLORIA-AF) registry. Am Heart J 2018;198:55–63.
62. Lee SR, Choi EK, Han KD, Jung JH, Oh S, Lip GYH. Edoxaban in Asian patients with atrial fibrillation: effectiveness and safety. J Am Coll Cardiol 2018;72:838–853.
63. Li XS, Deitelzweig S, Keshishian A, et al. Effectiveness and safety of apixaban versus warfarin in non-valvular atrial fibrillation patients in “real-world” clinical practice. A propensity-matched analysis of 76,940 patients. Thromb Haemost 2017;117:1072–1082.
64. Martínez CAA, Lanas F, Radaideh G, et al. XANTUS-EL: a real-world, prospective, observational study of patients treated with rivaroxaban for stroke prevention in atrial fibrillation in Eastern Europe, Middle East, Africa and Latin America. Egypt Heart J 2018;70:307–313.
65. Lee KH, Park HW, Lee N, et al. Optimal dose of dabigatran for the prevention of thromboembolism with minimal bleeding risk in Korean patients with atrial fibrillation. Europace 2017;19 Suppl 4:iv1–iv9.
66. Ingrasciotta Y, Crisafulli S, Pizzimenti V, et al. Pharmacokinetics of new oral anticoagulants: implications for use in routine care. Expert Opin Drug Metab Toxicol 2018;14:1057–1069.
67. Lee KH, Park HW, Cho JG, et al. Comparison of non-vitamin K antagonist oral anticoagulants and warfarin on clinical outcomes in atrial fibrillation patients with renal dysfunction. Europace 2015;17 Suppl 2:ii69–ii75.
68. Lee SR, Choi EK, Han KD, Jung JH, Oh S, Lip GYH. Optimal rivaroxaban dose in Asian patients with atrial fibrillation and normal or mildly impaired renal function. Stroke 2019;50:1140–1148.
69. Siontis KC, Zhang X, Eckard A, et al. Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States. Circulation 2018;138:1519–1529.
70. Stanton BE, Barasch NS, Tellor KB. Comparison of the safety and effectiveness of apixaban versus warfarin in patients with severe renal impairment. Pharmacotherapy 2017;37:412–419.
71. Steinberg BA, Shrader P, Thomas L, et al. Off-label dosing of non-vitamin K antagonist oral anticoagulants and adverse outcomes: the ORBIT-AF II Registry. J Am Coll Cardiol 2016;68:2597–2604.
72. Yao X, Shah ND, Sangaralingham LR, Gersh BJ, Noseworthy PA. Non-vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. J Am Coll Cardiol 2017;69:2779–2790.
73. Lee SR, Lee YS, Park JS, et al. Label adherence for non-vitamin K antagonist oral anticoagulants in a prospective cohort of Asian patients with atrial fibrillation. Yonsei Med J 2019;60:277–284.
74. Lee KN, Choi JI, Boo KY, et al. Effectiveness and safety of off-label dosing of non-vitamin K antagonist anticoagulant for atrial fibrillation in Asian patients. Sci Rep 2020;10:1801.
75. Cho MS, Yun JE, Park JJ, et al. Outcomes after use of standardand low-dose non-vitamin K oral anticoagulants in Asian patients with atrial fibrillation. Stroke 2018;50:110–118.
76. Joung B. Real-world data and recommended dosage of non-vitamin K oral anticoagulants for Korean patients. Korean Circ J 2017;47:833–841.
77. ACTIVE Writing Group of the ACTIVE Investigators, Connolly S, Pogue J, et al. Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation clopidogrel trial with irbesartan for prevention of vascular events (ACTIVE W): a randomised controlled trial. Lancet 2006;367:1903–1912.
78. ACTIVE Investigators, Connolly SJ, Pogue J, et al. Effect of clopidogrel added to aspirin in patients with atrial fibrillation. N Engl J Med 2009;360:2066–2078.
79. Själander S, Själander A, Svensson PJ, Friberg L. Atrial fibrillation patients do not benefit from acetylsalicylic acid. Europace 2014;16:631–638.
80. Lip GY. The role of aspirin for stroke prevention in atrial fibrillation. Nat Rev Cardiol 2011;8:602–606.
81. Mant J, Hobbs FD, Fletcher K, et al. Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation (the birmingham atrial fibrillation treatment of the aged study, BAFTA): a randomised controlled trial. Lancet 2007;370:493–503.
82. Holmes DR, Reddy VY, Turi ZG, et al. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial. Lancet 2009;374:534–542.
83. Reddy VY, Möbius-Winkler S, Miller MA, et al. Left atrial appendage closure with the Watchman device in patients with a contraindication for oral anticoagulation: the ASAP study (ASA plavix feasibility study with watchman left atrial appendage closure technology). J Am Coll Cardiol 2013;61:2551–2556.
84. Reddy VY, Doshi SK, Sievert H, et al. Percutaneous left atrial appendage closure for stroke prophylaxis in patients with atrial fibrillation: 2.3-year follow-up of the PROTECT AF (watchman left atrial appendage system for embolic protection in patients with atrial fibrillation) trial. Circulation 2013;127:720–729.
85. Holmes DR Jr, Kar S, Price MJ, et al. Prospective randomized evaluation of the watchman left atrial appendage closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. J Am Coll Cardiol 2014;64:1–12.
86. Boersma LV, Schmidt B, Betts TR, et al. Implant success and safety of left atrial appendage closure with the WATCHMAN device: peri-procedural outcomes from the EWOLUTION registry. Eur Heart J 2016;37:2465–2474.
87. Boersma LV, Ince H, Kische S, et al. Efficacy and safety of left atrial appendage closure with WATCHMAN in patients with or without contraindication to oral anticoagulation: 1-year follow-up outcome data of the EWOLUTION trial. Heart Rhythm 2017;14:1302–1308.
88. Badheka AO, Chothani A, Mehta K, et al. Utilization and adverse outcomes of percutaneous left atrial appendage closure for stroke prevention in atrial fibrillation in the United States: influence of hospital volume. Circ Arrhythm Electrophysiol 2015;8:42–48.
89. Pison L, Potpara TS, Chen J, et al. Left atrial appendage closure-indications, techniques, and outcomes: results of the European Heart Rhythm Association Survey. Europace 2015;17:642–646.
90. Price MJ, Gibson DN, Yakubov SJ, et al. Early safety and efficacy of percutaneous left atrial appendage suture ligation: results from the U.S. transcatheter LAA ligation consortium. J Am Coll Cardiol 2014;64:565–572.
91. Fauchier L, Cinaud A, Brigadeau F, et al. Device-related thrombosis after percutaneous left atrial appendage occlusion for atrial fibrillation. J Am Coll Cardiol 2018;71:1528–1536.
92. Lakkireddy D, Afzal MR, Lee RJ, et al. Short and long-term outcomes of percutaneous left atrial appendage suture ligation: results from a US multicenter evaluation. Heart Rhythm 2016;13:1030–1036.
93. van Laar C, Verberkmoes NJ, van Es HW, et al. Thoracoscopic left atrial appendage clipping: a multicenter cohort analysis. JACC Clin Electrophysiol 2018;4:893–901.
94. Healey JS, Crystal E, Lamy A, et al. Left atrial appendage occlusion study (LAAOS): results of a randomized controlled pilot study of left atrial appendage occlusion during coronary bypass surgery in patients at risk for stroke. Am Heart J 2005;150:288–293.
95. Whitlock RP, Vincent J, Blackall MH, et al. Left atrial appendage occlusion study II (LAAOS II). Can J Cardiol 2013;29:1443–1447.
96. Tsai YC, Phan K, Munkholm-Larsen S, Tian DH, La Meir M, Yan TD. Surgical left atrial appendage occlusion during cardiac surgery for patients with atrial fibrillation: a meta-analysis. Eur J Cardiothorac Surg 2015;47:847–854.
97. Aryana A, Singh SK, Singh SM, et al. Association between incomplete surgical ligation of left atrial appendage and stroke and systemic embolization. Heart Rhythm 2015;12:1431–1437.
98. Gillinov AM, Gelijns AC, Parides MK, et al. Surgical ablation of atrial fibrillation during mitral-valve surgery. N Engl J Med 2015;372:1399–1409.
99. Whitlock R, Healey J, Vincent J, et al. Rationale and design of the left atrial appendage occlusion study (LAAOS) III. Ann Cardiothorac Surg 2014;3:45–54.
100. Chao TF, Liu CJ, Lin YJ, et al. Oral anticoagulation in very elderly patients with atrial fibrillation: a nationwide cohort study. Circulation 2018;138:37–47.
101. Nielsen PB, Skjøth F, Søgaard M, Kjældgaard JN, Lip GY, Larsen TB. Effectiveness and safety of reduced dose non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ 2017;356:j510.
102. Larsen TB, Skjøth F, Nielsen PB, Kjældgaard JN, Lip GY. Comparative effectiveness and safety of non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ 2016;353:i3189.
103. Tilz RR, Potpara T, Chen J, et al. Left atrial appendage occluder implantation in Europe: indications and anticoagulation post-implantation. Results of the European Heart Rhythm Association Survey. Europace 2017;19:1737–1742.
104. Ogawa H, An Y, Ikeda S, et al. Progression from paroxysmal to sustained atrial fibrillation is associated with increased adverse events. Stroke 2018;49:2301–2308.
105. Potpara TS, Stankovic GR, Beleslin BD, et al. A 12-year follow-up study of patients with newly diagnosed lone atrial fibrillation: implications of arrhythmia progression on prognosis: the Belgrade atrial fibrillation study. Chest 2012;141:339–347.
106. Mahajan R, Perera T, Elliott AD, et al. Subclinical device-detected atrial fibrillation and stroke risk: a systematic review and meta-analysis. Eur Heart J 2018;39:1407–1415.
107. Brambatti M, Connolly SJ, Gold MR, et al. Temporal relationship between subclinical atrial fibrillation and embolic events. Circulation 2014;129:2094–2099.
108. Boriani G, Glotzer TV, Santini M, et al. Device-detected atrial fibrillation and risk for stroke: an analysis of >10,000 patients from the SOS AF project (stroke prevention strategies based on atrial fibrillation information from implanted devices). Eur Heart J 2014;35:508–516.
109. Freedman B, Camm J, Calkins H, et al. Screening for atrial fibrillation: a report of the AF-SCREEN international collaboration. Circulation 2017;135:1851–1867.
110. Freedman B, Boriani G, Glotzer TV, Healey JS, Kirchhof P, Potpara TS. Management of atrial high-rate episodes detected by cardiac implanted electronic devices. Nat Rev Cardiol 2017;14:701–714.
111. Camm AJ, Simantirakis E, Goette A, et al. Atrial high-rate episodes and stroke prevention. Europace 2017;19:169–179.
112. Boriani G, Glotzer TV, Ziegler PD, et al. Detection of new atrial fibrillation in patients with cardiac implanted electronic devices and factors associated with transition to higher device-detected atrial fibrillation burden. Heart Rhythm 2018;15:376–383.
113. Pastori D, Lip GYH, Farcomeni A, et al. Incidence of bleeding in patients with atrial fibrillation and advanced liver fibrosis on treatment with vitamin K or non-vitamin K antagonist oral anticoagulants. Int J Cardiol 2018;264:58–63.
114. Kuo L, Chao TF, Liu CJ, et al. Liver cirrhosis in patients with atrial fibrillation: would oral anticoagulation have a net clinical benefit for stroke prevention? J Am Heart Assoc 2017;6e005307.
115. Lee SR, Lee HJ, Choi EK, et al. Direct oral anticoagulants in patients with atrial fibrillation and liver disease. J Am Coll Cardiol 2019;73:3295–3308.
116. Staerk L, Lip GY, Olesen JB, et al. Stroke and recurrent haemorrhage associated with antithrombotic treatment after gastrointestinal bleeding in patients with atrial fibrillation: nationwide cohort study. BMJ 2015;351:h5876.
117. Eckman MH, Singer DE, Rosand J, Greenberg SM. Moving the tipping point: the decision to anticoagulate patients with atrial fibrillation. Circ Cardiovasc Qual Outcomes 2011;4:14–21.
118. Proietti M, Lip GY. Major S outcomes in atrial fibrillation patients with one risk factor: impact of time in therapeutic range observations from the PORTIF trials. Am J Med 2016;129:1110–1116.
119. Lip GY, Nielsen PB. Should Patients with atrial fibrillation and 1 stroke risk factor (CHA 2 DS 2 -VASc score 1 in men, 2 in women) be anticoagulated? Yes: even 1 stroke risk factor confers a real risk of stroke. Circulation 2016;133:1498–1503.
120. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on atrial fibrillation. Chest 2010;137:263–272.
121. Kim D, Yang PS, Kim TH, et al. Ideal blood pressure in patients with atrial fibrillation. J Am Coll Cardiol 2018;72:1233–1245.
122. Nielsen PB, Larsen TB, Skjøth F, Overvad TF, Lip GY. Stroke and thromboembolic event rates in atrial fibrillation according to different guideline treatment thresholds: a nationwide cohort study. Sci Rep 2016;6:27410.
123. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 2010;138:1093–1100.
124. Böhm M, Ezekowitz MD, Connolly SJ, et al. Changes in renal function in patients with atrial fibrillation: an analysis from the RE-LY trial. J Am Coll Cardiol 2015;65:2481–2493.
125. Hijazi Z, Hohnloser SH, Andersson U, et al. Efficacy and safety of apixaban compared with warfarin in patients with atrial fibrillation in relation to renal function over time: insights from the ARISTOTLE randomized clinical trial. JAMA Cardiol 2016;1:451–460.
126. Potpara TS, Polovina MM, Licina MM, Marinkovic JM, Prostran MS, Lip GY. Reliable identification of “truly low” thromboembolic risk in patients initially diagnosed with “lone” atrial fibrillation: the Belgrade atrial fibrillation study. Circ Arrhythm Electrophysiol 2012;5:319–326.
127. Weijs B, Dudink EAMP, de Vos CB, et al. Idiopathic atrial fibrillation patients rapidly outgrow their low thromboembolic risk: a 10-year follow-up study. Neth Heart J 2019;27:487–497.
128. Chao TF, Liao JN, Tuan TC, et al. Incident co-morbidities in patients with atrial fibrillation initially with a CHA 2 DS 2 -VASc score of 0 (males) or 1 (females): implications for reassessment of stroke risk in initially ‘low-risk’ patients. Thromb Haemost 2019;119:1162–1170.
129. Clarkesmith DE, Pattison HM, Lip GY, Lane DA. Educational intervention improves anticoagulation control in atrial fibrillation patients: the TREAT randomised trial. PLoS One 2013;8e74037.
130. Teiger E, Thambo JB, Defaye P, et al. Percutaneous left atrial appendage closure is a reasonable option for patients with atrial fibrillation at high risk for cerebrovascular events. Circ Cardiovasc Interv 2018;11e005841.
131. Hart RG, Pearce LA, Rothbart RM, McAnulty JH, Asinger RW, Halperin JL. Stroke with intermittent atrial fibrillation: incidence and predictors during aspirin therapy. Stroke prevention in atrial fibrillation investigators. J Am Coll Cardiol 2000;35:183–187.
132. Saw J, Fahmy P, Azzalini L, et al. Early Canadian multicenter experience with WATCHMAN for percutaneous left atrial appendage closure. J Cardiovasc Electrophysiol 2017;28:396–401.
133. Martin Gutierrez E, Castano M, Gualis J, et al. Beneficial effect of left atrial appendage closure during cardiac surgery: a meta-analysis of 280 585 patients. Eur J Cardiothorac Surg 2020;57:252–262.
심방세동 치료 가이드라인
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License ( http://creativecommons.org/licenses/by- nc/3.0/ ) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia in the general population. The Korean Heart Rhythm Society organized a Korean Atrial Fibrillation Management Guideline Committee and analyzed all available studies regarding the management of AF, including studies on Korean patients. This guideline is based on recent data of the Korean population and the recent guidelines of the European Society of Cardiology, European Association for Cardio-Thoracic Surgery, American Heart Association, and Asia Pacific Heart Rhythm Society. Expert consensus or guidelines for the optimal management of Korean patients with AF were achieved after a systematic review with intensive discussion. This article provides general principles for appropriate risk stratification and selection of anticoagulation therapy in Korean patients with AF. This guideline deals with optimal stroke prevention, screening, rate and rhythm control, risk factor management, and integrated management of AF.
심방세동 치료 가이드라인
심방세동 치료 가이드라인
Guideline of atrial fibrillation management
정보영 | 연세대학교 의과대학 세브란스병원 심장내과
서론
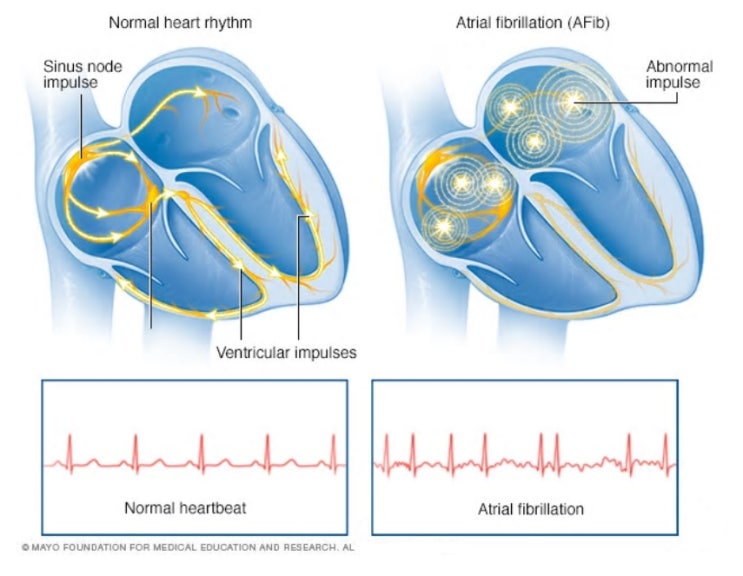
심장부정맥은 심장 리듬이 흐트러지는 병으로 뇌졸중, 급사 등 심각한 질환과 연관이 되어있다. 부정맥 중 특히 심방세동은 가장 흔하고 고령화로 전 세계적으로 유병률이 증가되고 있다. 국내에서도 최근 고령화로 인해 심방세동 환자가 더욱 뚜렷한 증가 추세를 보이고 있다.
심방세동은 특히 뇌졸중의 위험도를 약 4배 정도 올리지만 아직까지 국내 심방세동 환자의 항응고요법 사용률은 30% 미만으로 낮은 실정이다. 최근 보고된 삼차병원의 항응고요법 사용률은 83% 정도로 높은 수준을 유지함에 비하여 일차, 이차 기관의 항응고요법은 더욱 낮아서 심방세동 환자의 질환 관리에 대한 일차, 이차 의료기관 교육 및 협력의 중요성이 더욱 커지고 있다.
2018년 부정맥학회에서 발표한 ‘심방세동 치료 가이드라인’은 급속도로 증가하고 있는 심방세동 및 최근 도입된 비타민 K 비의존성 항응고제(non-vitamin K antagonist oral anti-coagulants, NOAC)를 고려하여 뇌졸중 예방의 중요성을 강조하고 심방세동 치료를 위하여 의료기관들의 협력이 요구되는 새로운 의료환경 변화에 대응하고자 개발되었다.
= 중 략 =
So you have finished reading the 심방 세동 치료 가이드 라인 topic article, if you find this article useful, please share it. Thank you very much. See more: 심방세동 완치율, 심방세동 관리, 심방세동 응급처치, 심방세동 심부전, 심방세동 진단기준, 심방세동 종류, 심방세동 심전도, Atrial fibrillation Guideline

